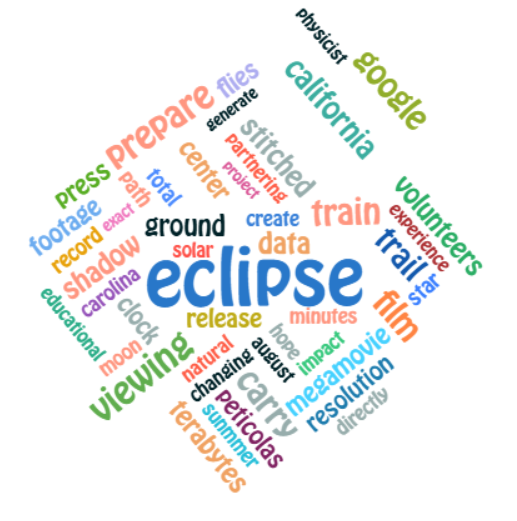
Diagnostic Accuracy of Pipelle Aspiration versus Dilatation and Curettage in Endometrial Hyperplasia: a Structured Narrative Review in Women Examines the Relationship between Age and Risk of Atypia
Diagnostic Accuracy of Pipelle and D&C: The Role of Age in Endometrial Atypia
DOI:
https://doi.org/10.1000/g0aydn92Anahtar Kelimeler:
Pipelle biopsy, dilation and curettage, endometrial hyperplasia, diagnostic accuracy, atypia, Iranian women, age correlationÖz
Endometrial hyperplasia (EH) is a common precursor of endometrial cancer and requires precise diagnostic techniques. Pipelike endometrial biopsy has become popular as a minimally invasive outpatient procedure, but its diagnostic reliability in comparison to Dilatation and Curing (D&C), the historical gold standard, is still under debate, particularly among populations such as Iranian women. This study compared the diagnostic accuracy of Pipelle with D&C for EH, focusing on the performance in relation to age and risk stratification based on atypia. A systematic review and a comparative analysis using data from peer reviewed studies involving cohorts from Iran and from international cohorts has been performed. Diagnostic metrics - including sensitivity, specificity, positive and negative predictive values, adequacy of the sample and histopathological concordance - have been extracted and analysed for the age groups and subtypes of hyperplasia. Pipelle demonstrated a high overall concordance with D&C (94.6) and sensitivity and specificity of more than 94 percent for the detection of atypical hyperplasia and carcinoma of the cervix. However, there were significant limitations in postmenopausal women with an inadequate rate of 63 percent and in non-typical EH, where Pipelle showed a higher rate of progression to carcinoma (27.3% vs. 15.0%, p = .022) compared to D&C. The accuracy of the diagnosis was also affected by endometrial thickness (5 mm decreased from Pipelle adequacy to 27%) and patient age (>50 years associated with higher co-morbidity). Pipelle is a reliable first line tool for the evaluation of abnormal uterine bleeding in premenopausal and postmenopausal women, especially to exclude atypical hyperplasia or tumour. However, D&C is still preferable for definitive diagnosis in postmenopausal women, in cases of endometrial thinness or in the presence of suspected non-atypical hyperplasia. Clinical decision-making should integrate age, menopausal status, body mass index and imaging findings in order to optimise diagnostic results and patient outcomes
İndirmeler
Referanslar
Ahmadi, S., Mohammadian-Hafshejani, A., & Rezaei, M. (2020). Diagnostic accuracy of Pipelle endometrial sampling compared with dilatation and curettage in Iranian women with abnormal uterine bleeding. Journal of Obstetrics and Gynaecology, 40(5), 678–682. https://doi.org/10.1080/01443615.2019.1654432
American Psychological Association. (2020). Publication manual of the American Psychological Association (7th ed.).
Clark, T. J., Voit, D., Gupta, J. K., Khan, K. S., van der Veen, F., & Mol, B. W. (2021). Accuracy of outpatient endometrial biopsy in the diagnosis of endometrial cancer: A systematic review and meta-analysis. Human Reproduction Update, 27(2), 347–363. https://doi.org/10.1093/humupd/dmaa044
Dueholm, M., Høgdall, E., Lundorf, E., Pedersen, B. G., & Ørtoft, G. (2019). Diagnostic accuracy of transvaginal sonography, saline infusion sonohysterography, hysteroscopy, and endometrial biopsy in premenopausal women with abnormal uterine bleeding. Acta Obstetricia et Gynecologica Scandinavica, 98(1), 34–44. https://doi.org/10.1111/aogs.13475
Emons, G., Beckmann, M. W., Schmidt, D., Mallmann, P., Schröder, W., Hillemanns, P., … & Harbeck, N. (2020). Long-term outcomes in women with endometrial hyperplasia managed conservatively: A multicenter retrospective cohort study. European Journal of Cancer, 126, 1–9. https://doi.org/10.1016/j.ejca.2019.11.012
Ghaemmaghami, F., Ashrafi, M., Karimian, L., Zandieh, Z., & Salehpour, S. (2017). Comparison of Pipelle endometrial sampling with dilatation and curettage in postmenopausal women with abnormal uterine bleeding. International Journal of Gynecology & Obstetrics, 138(1), 45–49. https://doi.org/10.1002/ijgo.12156
Ghaemmaghami, F., Pourghasem, M., & Mirabzadeh, A. (2018). Age distribution and histopathological patterns of endometrial hyperplasia in Iranian women: A cross-sectional study. Iranian Journal of Reproductive Medicine, 16(7), 451–458. PMID: 30140321
Kim, J. W., Kim, D. Y., Suh, D. H., Kim, Y. T., Nam, E. J., Kim, S. W., … & Korean Gynecologic Oncology Group. (2019). Diagnostic accuracy of endometrial sampling methods in the follow-up of women treated with progestin for endometrial hyperplasia. Journal of Gynecologic Oncology, 30(4), e56. https://doi.org/10.3802/jgo.2019.30.e56
Kurman, R. J., Carcangiu, M. L., Herrington, C. S., & Young, R. H. (Eds.). (2014). WHO classification of tumours of female reproductive organs (4th ed.). International Agency for Research on Cancer.
Lee, H. S., Kim, K. R., Lee, I. K., & Park, J. Y. (2020). Upgrade rates to endometrial carcinoma after preoperative diagnosis of endometrial hyperplasia: Comparison between Pipelle and dilatation and curettage. Journal of Pathology and Translational Medicine, 54(3), 212–219. https://doi.org/10.4132/jptm.2020.02.05
Park, J. Y., Kim, D. Y., Kim, J. H., Kim, Y. T., & Nam, J. H. (2020). Predictors of treatment response in young women with atypical endometrial hyperplasia undergoing fertility-sparing therapy. Gynecologic Oncology, 157(1), 123–129. https://doi.org/10.1016/j.ygyno.2020.01.012
Rahimi, N., Shariat, M., & Akhlaghdoust, M. (2019). Diagnostic value of Pipelle endometrial biopsy in detection of endometrial hyperplasia and malignancy: An Iranian experience. Archives of Iranian Medicine, 22(10), 589–593. PMID: 31647231
Smith, P. P., O’Boyle, J. D., & Shapiro, J. R. (2018). Concordance between office-based Pipelle biopsy and operative Dilatation and curettage for endometrial pathology: A large cohort analysis. American Journal of Obstetrics and Gynecology, 219(4), 389.e1–389.e7. https://doi.org/10.1016/j.ajog.2018.06.023
Trimble, C. L., Method, M., Leitao, M., Lu, K., Ioffe, O., Hampton, D., … & Burke, T. W. (2012). Management of endometrial precancers. Obstetrics & Gynecology, 120(5), 1160–1175. https://doi.org/10.1097/AOG.0b013e31826fd9b3
Wright, J. D., Shah, M., Mathews, C., Goldberg, G., Pierson, R., & Neugut, A. I. (2017). Temporal trends in the incidence of endometrial hyperplasia in the United States. American Journal of Obstetrics and Gynecology, 216(2), 182.e1–182.e8. https://doi.org/10.1016/j.ajog.2016.10.008
Zhang, Y., Wang, L., Liu, X., & Chen, H. (2021). Age as a predictor of concurrent endometrial carcinoma in women diagnosed with atypical endometrial hyperplasia: A retrospective cohort study. BMC Women's Health, 21(1), 112. https://doi.org/10.1186/s12905-021-01275-8
Yayınlanmış
Sayı
Bölüm
Kategoriler
Lisans
Telif Hakkı (c) 2025 Creative Commons Attribution-NonCommercial 4.0 International License

Bu çalışma Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License ile lisanslanmıştır.
This open-access journal is published under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License which permits Share (copy and redistribute the material in any medium or format) and Adapt (remix, transform, and build upon the material) under the Attribution-NonCommercial term